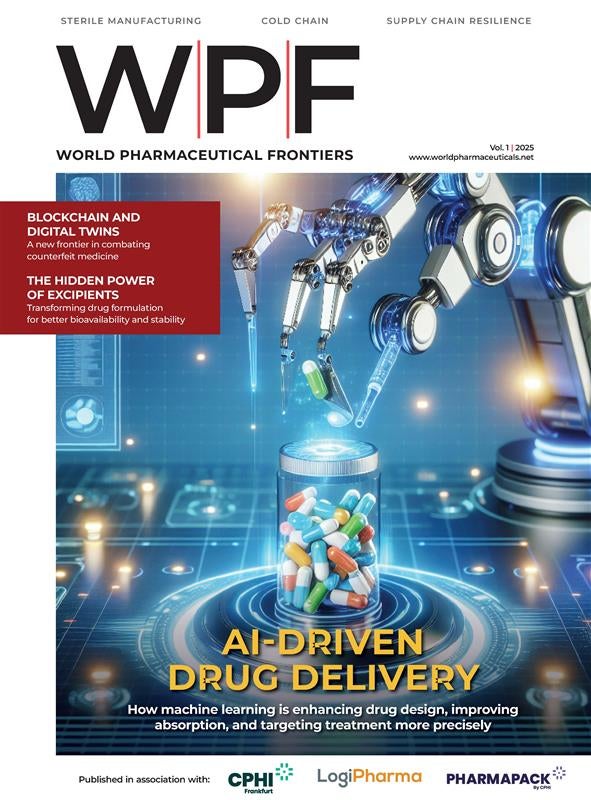
World Pharmaceutical Frontiers
WPF
Why is World Pharmaceutical Frontiers essential reading?
The pharmaceutical industry is changing faster than ever before. Regulations are becoming more demanding, and there are more technologies, faster product launches and shorter product life cycles. At the same time the cost of R&D is continuously increasing. This is putting heavier financial pressure on pharma to reduce costs and shorten lead times without compromising quality or patient safety, and choosing the right investment has never been more essential.
World Pharmaceutical Frontiers is the premier information source for the world’s leading pharmaceutical companies, with reliable and accurate intelligence on emerging trends and breakthrough technologies to help them make critical business decisions.
Focusing on all areas of the pharmaceutical industry and aimed at senior executives in charge of purchasing, R&D and manufacturing, World Pharmaceutical Frontiers provides a clear overview of the latest industry thinking regarding pharma and is essential reading for those who want to stay ahead of the competition.
Communicate directly with the Pharma community
We continue to invest heavily in the circulation of World Pharmaceutical Frontiers and have created a powerful international readership. Our database of key decision-makers in the pharmaceutical industry accounts for approximately 72% of all purchasing authority.
World Pharmaceutical Frontiers has an ABC audited circulation and a projected readership of over 49,000 (publisher’s survey).
World Pharmaceutical Frontiers reaches a target audience of industry peers with the highest levels of purchasing and decision-making power, including the top decision-makers in the buying chain at the top 50 pharmaceutical and biotechnology companies worldwide, as well as leading CROs and CMOs.
Geo Splits

Target Job function

Level of purchasing involvement

Representative job titles
- VP Manufacturing
- CEO
- Business Unit Manager
- Quality Control Director
- Managing Director
- Technical Director
- Head of Operations
- President
- Chief Scientific Officer
- Head of Production
- VP of Licensing
- Formulation Director
- Director of R&D
- Innovation Director
- Head of Food Engineering
- Head of Supply Chain
- VP of Purchasing
- Procurement Manager
Our readers include professionals from:

Newsletter:
Each week the World Pharma newsletter is sent out to 20,000 digital readers. Covering the latest pharmaceutical manufacturing news from product development, clinical trials, manufacturing, supply chain, outsourcing and regulatory compliance. The newsletter recipients also receive the latest digital version of the magazine also.
We manage the ‘World pharma frontiers forum group on LinkedIn which is a specialist network of about 200 (and counting) pharmaceutical professionals. With regular posts and updates, as well as the latest industry data, it is a great way to engage the sector.
Distribution